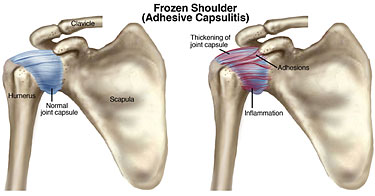
Frozen Shoulder (Adhesive Capsulitis)
Frozen shoulder is a very painful condition involving the shoulder. Frozen shoulder is also known as Adhesive Capsulitis. The condition involves inflammation and thickening of the joint capsule, or the sack that surrounds the shoulder joint. As the capsule becomes inflamed and thickened, it hurts to move in any direction. The hallmark of the condition is worsening stiffness, and loss of motion in every direction. Frozen shoulder has 3 stages: 1) a painful stage, 2) a frozen stage, and 3) a thawing stage. The first stage is very painful and the shoulder has worsening stiffness. Symptoms include pain that is worse with any movement, any stretching, and pain at night. In the second stage, the pain goes away but the shoulder remains very stiff. It becomes difficult to raise the arm up or reach behind the back. In the third stage, the stiffness slowly resolves. Frozen shoulder is a very common condition in the shoulder.
How does this happen?
A frozen shoulder can be caused by many factors, including trauma, an injury to the shoulder, lifting something heavy, and repetitive overhead activities. After an injury, it may hurt to move the shoulder, and immobilization makes the shoulder stiff. In many cases, there is no injury, and the pain and stiffness slowly worsen over time. Frozen shoulder is more common in women and in people with diabetes and thyroid disorder. If you do nothing, it should resolve on its own over time, but this may take up to 2 years. Treatment options are available to help speed up this process.
How will we know that this is your problem?
The diagnosis of adhesive capsulitis (frozen shoulder) is made by a physician through a combination of history and physical exam. The history may include a specific injury, but more commonly pain and stiffness develop slowly over time without a traumatic injury. Examination of the shoulder confirms the diagnosis, with stiffness (loss of motion) in every direction and pain with stretching. X-rays are often completely normal. An MRI of the shoulder may be obtained to evaluate for thickening and inflammation in the capsule and to rule out a rotator cuff tear.
How can this be treated?
The initial treatment for a frozen shoulder is a cortisone injection into the shoulder joint and anti-inflammatory pain medication (NSAID’s) to decrease pain and inflammation. The mainstay of treatment involves physical therapy and daily home stretches to stretch the joint capsule and regain range of motion. Once motion improves, therapy progresses to strengthening. The cortisone injection is very helpful because it decreases the pain to allow you to complete physical therapy. When non-operative treatment fails to provide pain relief, surgery may be necessary. Current thinking is to avoid a Manipulation Under Anesthesia, as this may result in damage to the soft tissue structures of the shoulder, such as a rotator cuff tear. Surgery can be performed arthroscopically (using a scope) to release the capsule and remove scar tissue from the shoulder joint. This surgery is called a Capsular Release, and is precise and safe. Following surgery, patients must resume physical therapy the very next day to keep the shoulder moving. Surgery is typically performed as an outpatient, and you can go home the same day.
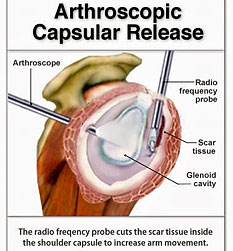
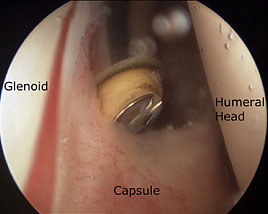
Dr. Michael O’Brien performs arthroscopic surgery for adhesive capsulitis. He is board certified and fellowship trained in the field of shoulder surgery and shoulder reconstruction. Dr. O’Brien has tremendous success in improving patients’ pain and range of motion and returning them to their normal activities with arthroscopic capsular release.
The Tulane Institute of Sports Medicine offers on-site X-Ray and MRI, as well as its own Physical Therapy department with licensed physical therapists and a pool, in order to ease your visit and speed your recovery.
